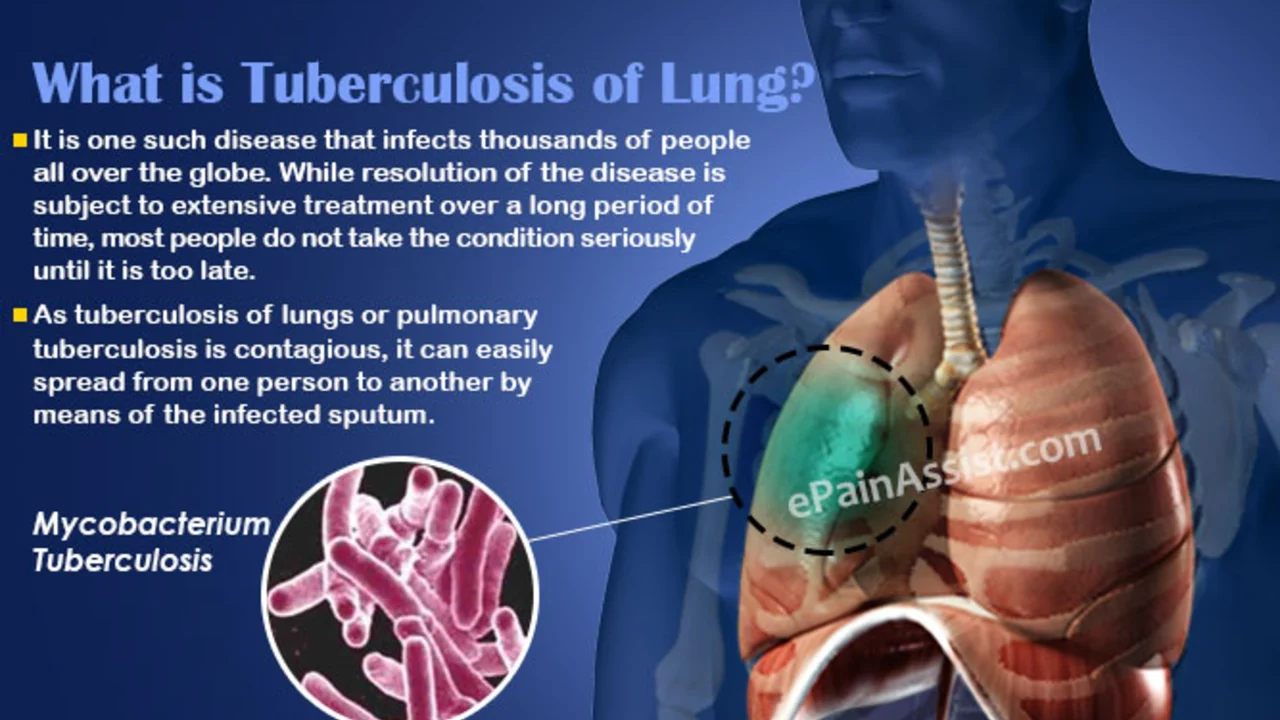
Drug-Resistant Tuberculosis: A Growing Global Concern
As a concerned global citizen, I can't ignore the alarming increase in cases of drug-resistant tuberculosis (TB). My latest post delves into this growing global health worry, explaining why the rise in drug-resistant TB is particularly ominous. It discusses the various factors contributing to its spread and the challenges it poses to the medical community in treating it. We all should be aware of this urgent issue, as it may affect us directly or indirectly. So, join me as we take a closer look at this critical matter.
Read more